Healthcare is in the middle of a data revolution with drastic regulation changes and technological improvements very day. Every patient encounter, lab test, prescription, and image produces digital information that can improve care and save lives. Yet, more than 37% of healthcare leaders surveyed by HIMSS in 2024 struggled to leverage data in decision making because of integration and onboarding challenges including resource constraints. Without healthcare data accessibility, the promise of digital health remains out of reach. For a comprehensive resource that covers how your healthcare organization can achieve data accessibility—examining the regulations shaping it, the technologies driving progress, the outcomes it delivers, and the emerging trends poised to transform its future—this guide is for you.
What Is Healthcare Data Accessibility?
Healthcare data accessibility means that the right people can securely access the right patient data at the right time. It goes beyond storage—it’s about ensuring that data is usable, shareable, and available to support clinical decisions, improve patient experience, and drive innovation.
Accessibility is more than convenience. It’s a core requirement for:
-
Patient safety: Clinicians need complete and accurate records to avoid errors.
-
Continuity of care: Providers across different settings must be able to see the same patient history.
-
Research and innovation: Accessible datasets fuel medical research, clinical trials, and population health insights.
-
Operational efficiency: Organizations can reduce costs and administrative burden when data flows freely.
In short, healthcare data accessibility is the foundation of modern care delivery.
Why Healthcare Data Accessibility Matters
Regulations Driving Data Accessibility
Several major regulations and frameworks set the parameters for what constitutes healthcare data accessibility and how it must be achieved. These not only define who should have access to patient information and under what circumstances, but also establish technical and operational standards to ensure data is available, interoperable, and secure across the healthcare ecosystem. Compliance with these regulations is fundamental—failure to adhere can result in legal, financial, and reputational risks. As industry demands evolve, these frameworks provide the foundation for secure patient data sharing, enabling innovation while safeguarding privacy and advancing the quality of care.
The 21st Century Cures Act
The Cures Act (2016) requires healthcare providers, developers, and health information networks to give patients secure access to their health information. Key provisions include:
-
Prohibiting information blocking.
-
Mandating APIs for patient access.
-
Promoting interoperability across systems.
TEFCA (Trusted Exchange Framework and Common Agreement)
TEFCA establishes a nationwide data-sharing framework that sets the rules for how health information networks exchange data. Its goals:
-
Create a single “on-ramp” for providers, payers, and patients.
-
Standardize technical and governance requirements.
-
Expand patient access and system interoperability.
USCDI (United States Core Data for Interoperability)
The USCDI defines the standardized set of health data classes (e.g., demographics, allergies, medications, clinical notes) that must be shared across systems. Each new version expands what data must be accessible.
Together, these rules and frameworks ensure that healthcare data accessibility is not optional but a legal and operational necessity.
Technology Enablers of Healthcare Data Accessibility
To meet regulatory demands and clinical needs, organizations rely on an expanding ecosystem of technology solutions and vendors designed to enable secure data exchange, support evolving compliance requirements, and address the complexities of modern care delivery. These tools span the entire data lifecycle—from capture and standardization at point-of-care to integration, storage, and long-term archival—empowering healthcare providers to streamline workflows, enhance interoperability, and maintain robust data governance. By leveraging leading-edge platforms and purpose-built technologies, health systems are better equipped to facilitate clinician access, protect patient privacy, and adapt to both regulatory changes and operational shifts with agility.
Electronic Health Records (EHRs)
The backbone of healthcare data accessibility, but often siloed. Modern EHRs are evolving to support open APIs and FHIR standards.
APIs and FHIR (Fast Healthcare Interoperability Resources)
APIs based on the FHIR standard allow secure, structured data exchange between systems and apps. They are the key enabler of patient-facing applications.
Cloud-Based Solutions
Cloud platforms improve accessibility by allowing secure, scalable storage and data exchange beyond local servers.
Health Information Exchanges (HIEs)
HIEs aggregate data from multiple providers and systems, making records available across networks.
Data Migration and Archiving Tools
Solutions for transitioning data from one vendor to another or storing with access from your EHR ensure that legacy data remains accessible during EHR transitions or system decommissioning.
Data Lakes and Analytics Platforms
Enterprise-scale data lakes integrate multiple datasets for advanced analytics, population health, and research.
Disaster Recovery and Business Continuity
Cloud-based disaster recovery tools ensure uninterrupted data access during outages or cyber incidents.
Outcomes of Improving Data Accessibility
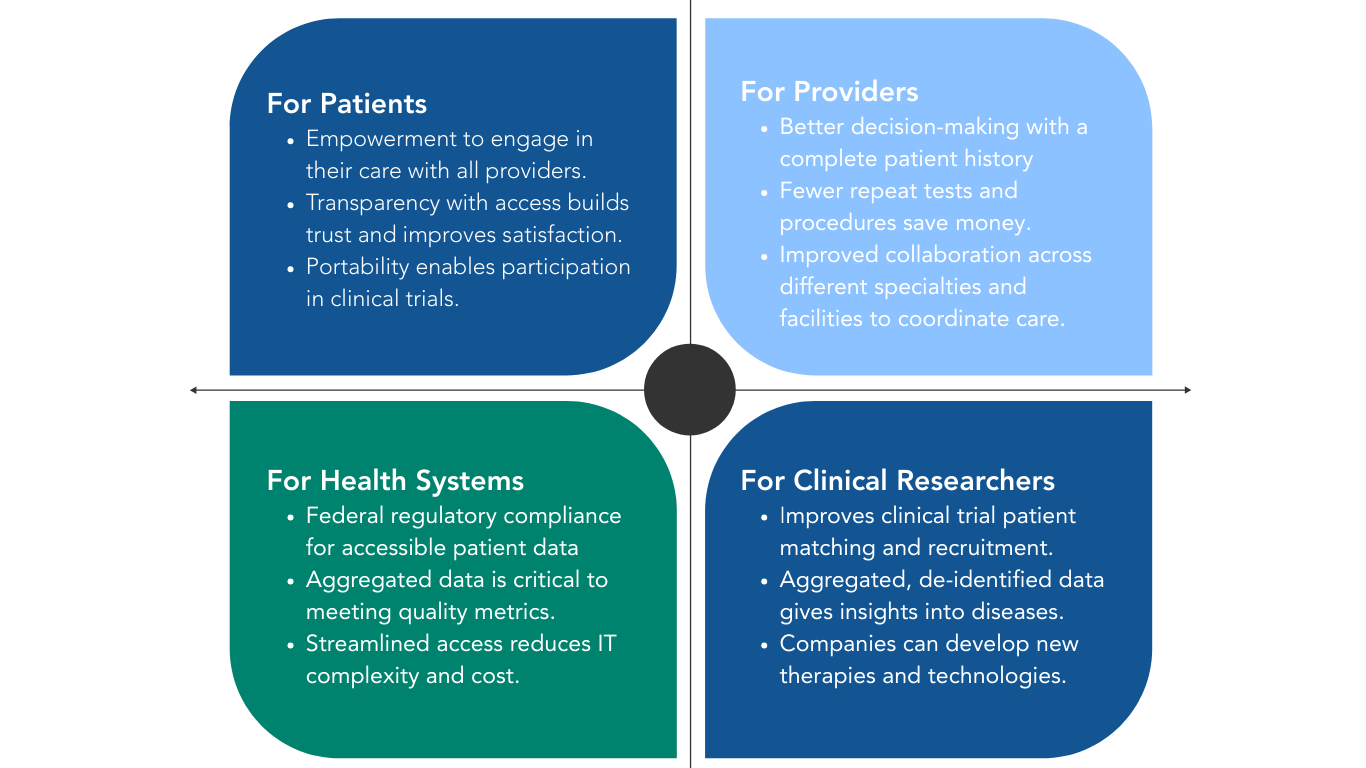
Improving healthcare data accessibility is not only about compliance—it leads to measurable, organization-wide benefits that directly impact clinical, operational, financial, and patient outcomes. Some example measurable outcomes:
-
Clinical outcomes: Reduced medical errors, faster diagnoses, improved chronic disease management.
-
Operational outcomes: Lower costs from reduced duplicate tests, streamlined workflows, and better resource use.
-
Financial outcomes: Increased revenue capture, improved coding accuracy, stronger reimbursement alignment.
-
Patient outcomes: Greater engagement, higher satisfaction, and better health literacy.
-
Research outcomes: Faster clinical trial enrollment, stronger evidence generation, and accelerated innovation.
Future Trends in Healthcare Data Accessibility
The last 18 months has seen drastic evolutions in technology and adoption with the introduction of AI. New solution providers are comping to market addressing many aspects of healthcare organizations biggest pain points. Yet, new healthcare innovations are useless or unable to reach their true potential without integration and aggregation for data accessibility. The next decade will see dramatic changes in how healthcare data is stored, shared, and used. Here are some areas Hart expects significant evolution in the months and years ahead:
AI and Machine Learning
AI depends on large, accessible datasets. As accessibility improves, predictive analytics and clinical decision support will become more powerful.
Patient-Centered Apps
Consumer health apps will continue to expand, giving patients more control over their data and integrating it with wearables and remote monitoring.
National Health Data Networks
TEFCA will evolve into a robust national network where patients, providers, payers, and researchers can securely exchange data.
Cross-Sector Data Sharing
Beyond healthcare, accessibility will expand to include social determinants of health, payers, and even retail and consumer data.
Advanced Security and Privacy Models
As access expands, so will the need for advanced consent management, de-identification, and cybersecurity solutions.
Related Topics
Explore deeper insights to achieving healthcare data accessibility for your organization:
-
EHR Data Migration: Ensuring Accessibility Through Transitions
-
Interoperability Standards: From HL7 to FHIR
Take your next step to improve data access
Healthcare data accessibility is no longer optional—it is the cornerstone of modern care, compliance, and innovation. By understanding the regulatory landscape, leveraging the right technology, and focusing on outcomes, healthcare organizations can unlock the full potential of their data.
This guide provides the foundation. The future belongs to organizations that put healthcare data accessibility at the center of their strategy.
-1.png?width=182&height=100&name=logo%20main%20blue%20(1)-1.png)